
What Is Coronary Artery Disease?
Coronary artery disease (CAD) occurs when the arteries that supply blood to the heart muscle (the coronary arteries) become hardened and narrowed. The arteries harden and narrow due to buildup of a material called plaque (plak) on their inner walls. The buildup of plaque is known as atherosclerosis (ATH-er-o-skler-O-sis). As the plaque increases in size, the insides of the coronary arteries get narrower and less blood can flow through them. Eventually, blood flow to the heart muscle is reduced, and, because blood carries much-needed oxygen, the heart muscle is not able to receive the amount of oxygen it needs. Reduced or cutoff blood flow and oxygen supply to the heart muscle can result in:
* Angina (AN-ji-na or an-JI-na). Angina is chest pain or discomfort that occurs when the heart does not get enough blood.
* Heart attack. A heart attack happens when a blood clot develops at the site of plaque in a coronary artery and suddenly cuts off most or all blood supply to that part of the heart muscle. Cells in the heart muscle begin to die if they do not receive enough oxygen-rich blood. This can cause permanent damage to the heart muscle.
Over time, CAD can weaken the heart muscle and contribute to:
* Heart failure. In heart failure, the heart can’t pump blood effectively to the rest of the body. Heart failure does not mean that the heart has stopped or is about to stop. Instead, it means that the heart is failing to pump blood the way that it should.
* Arrhythmias (a-RITH-me-as). Arrhythmias are changes in the normal beating rhythm of the heart. Some can be quite serious.
CAD is the most common type of heart disease. It is the leading cause of death in the United States in both men and women.
Heart disease is also referred to as coronary artery disease, atherosclerosis, atherosclerotic heart disease or hardening of the arteries. It is a condition in which fatty substances gradually build up in your blood vessels, causing the vessels to become more narrow and restricting the flow of blood through the vessel. This buildup is common in the small arteries of the heart, brain, kidneys, legs and neck.
The arteries in your heart (coronary arteries), which are about the size of a strand of spaghetti, are blood vessels that carry oxygen and nutrients that feed the heart muscle. At birth the inside walls of the arteries are smooth, like the inside walls of a new water pipe, allowing blood to flow easily through the vessel.
Just as water pipes may gradually develop a buildup of minerals and debris on the inside surface causing the water to flow more slowly, the arteries may gradually develop a buildup of plaque on the inside surface of the arteries, restricting the blood flow. Plaque is made up of cholesterol, which is fatty deposits, and fibrous tissue, which is scar tissue that forms where an artery has been damaged. Plaque may have begun to build up in your arteries when you were young; however you may not notice any problems or effects until later in life. Usually symptoms begin when there is at least a 75 percent blockage in your artery. Plaque may also build up in more than one place in your artery.
The narrowings that result from the buildup of plaque in heart disease are also known as plaques, lesions, clogged areas, atherosclerosis and arteriosclerosis. When plaque builds up, it restricts the flow of blood to the heart, thereby restricting the amount of oxygen and nutrients that the heart receives from the blood. If you increase your heart activity with any exercise, exertion or mental or emotional stress, you are increasing your heart' s need for oxygen, which is already in limited supply. If the heart does not receive enough oxygen, it is experiencing ischemia, which may cause heart pain known as angina or a heart attack.
Symptoms of Coronary Artery Disease
The amount of buildup and the location of the blockages determine the symptoms you will experience when you have heart disease (coronary artery disease/atherosclerosis). Symptoms of heart disease include angina and heart attacks. Each of these has its own symptoms as well.
If you have experienced the symptoms of heart disease, such as chest pain, shortness of breath or dizziness, you should consult your physician. There are several tests your physician can run to help diagnose coronary artery disease, as well as the severity of the disease, if you are found to have it. Your physician may run one or more tests. Click on one of the tests listed in the more info section for a more detailed description of each procedure, as well as information about preparation, length and the effects of each test.
Coronary Artery Causes, Incidence, and Risk Factors:
Coronary heart disease (CHD) is the leading cause of death in the United States for men and women. According to the American Heart Association, about every 29 seconds someone in the U.S. suffers from a CHD-related event, and about every minute someone dies from one.
The lifetime risk of having CHD after age 40 is 49% for men and 32% for women. As women get older, the risk increases almost to that of men. (See also heart disease and women.)
There are many factors that increase the risk for CHD. Some of the risks are based on family history (genetics), and others are more controllable. Risk factors include:
* Family history of coronary heart disease (especially before age 50)
* Male gender
* Age (65 and greater)
* Tobacco smoking
* High blood pressure
* Diabetes
* High cholesterol levels (specifically, high LDL cholesterol and low HDL cholesterol)
* Lack of physical activity or exercise
* Obesity
* High blood homocysteine levels
* Menopause in women
* Infection that causes inflammation in the artery wall. (There is some evidence that suggests this, but the theory is being studied.)
Coronary Artery Treatments
Regulate your cholesterol levels.
Cholesterol levels are one of the most modifiable risk factors you could have for developing atherosclerosis and coronary artery disease.
Ideally, you would want your total cholesterol levels to be below 200 mg/dL and your LDL cholesterol levels to be below 100 mg/dL (the new guidelines designate that certain high risk individuals should have this number at or lower than 70 mg/dL. Your HDL cholesterol (also known as the "good" cholesterol) should be above 40 mg/dL. Having high levels of HDL is a good thing, since it can exert a cardioprotective effect. Research has shown that aggressively treating cholesterol levels may prevent heart disease.
Stop smoking!
Many correlate smoking with lung cancer, however, nicotine addiction can be closely linked to another significant condition: heart disease. Smoking raises LDL cholesterol, lowers HDL cholesterol, and increases platelet aggregation. When this is coupled with the irritation smoking exerts on the arterial lining, it is a recipe for a potential disaster. According to the World Health Organization, you could cut your risk of CHD by half after quitting for one year, and with each subsequent year, your risk drops lower.
Check your blood pressure
Hypertension is a silent killer that also places you at risk for heart disease. Many people do not know they have high blood pressure until a routine visit to their health care practitioner. It doesn't necessarily affect cholesterol levels, but if it is ignored its effects can be deadly.
Eat healthy
Maintaining a healthy diet plays an important role in good heart health. This would include consuming a diet high in whole grains, fiber, fruits, and vegetables while limiting your consumption of saturated fats and trans fats (these are fats found in many cookies and snack foods).
Get some exercise.
Your heart is a muscle and exercise can benefit this. Moderate exercise can raise HDL levels, lower LDL levels, lower blood pressure, and prevent weight gain. During the week, you should exercise about 30 minutes 5 to 6 days out of the week. Even if you are not a marathon runner or a gymnast, you would be surprised how much benefit you can derive out of running up those steps instead of taking the elevator, or taking a brisk walk on a nice day.
Lose weight
If you are obese, losing 5-10% of your body weight can improve your cholesterol levels. Being overweight places you at risk for not only high cholesterol levels, but also type II diabetes mellitus. These two conditions are major risk factors for developing heart disease. By controlling your weight, you are also controlling your cholesterol and helping your heart to stay healthy.
How Is Coronary Artery Disease Treated ?
Treatment for coronary artery disease (CAD) may include lifestyle changes, medicines, and special procedures. The goals of treatment are to:
* Relieve symptoms
* Slow or stop atherosclerosis by controlling or reducing the risk factors
* Lower the risk of having blood clots form, which can cause a heart attack
* Widen or bypass clogged arteries
Lifestyle Changes
Making lifestyle changes can help treat CAD. For some people, these changes may be the only treatment needed:
* Eat a healthy diet to prevent or reduce high blood pressure and high blood cholesterol and to maintain a healthy weight
* Quit smoking, if you smoke
* Exercise, as directed by your doctor
* Lose weight, if you are overweight or obese
* Reduce stress
Coronary Artery Medicines
In addition to making lifestyle changes, medicines may be needed to treat CAD. Some medicines decrease the workload on the heart and relieve symptoms of CAD. Others decrease the chance of having a heart attack or dying suddenly and prevent or delay the need for a special procedure (for example, angioplasty or bypass surgery).
Several types of medicine are commonly used to treat CAD.
* Cholesterol-lowering medicines help to reduce your cholesterol to a doctor-recommended level.
* Anticoagulants (AN-te-ko-AG-u-lant) help to prevent clots from forming in your arteries and blocking blood flow.
* Aspirin, and other antiplatelet medicines, help to prevent clots from forming in your arteries and blocking blood flow. Blood contains small cells called platelets which clump together to form clots. Antiplatelet medicines reduce the ability of platelets to form clots. Aspirin may not be appropriate for some people because it increases the risk of bleeding. Discuss the benefits and risks with your doctor before starting aspirin therapy.
* ACE (angiotensin-converting enzyme) inhibitors help to lower blood pressure and reduce strain on your heart. They also may reduce the risk of a future heart attack and heart failure.
* Beta blockers slow your heart rate and lower your blood pressure to decrease the workload on your heart. Beta blockers are used to relieve angina and may also reduce the risk of a future heart attack.
* Calcium channel blockers relax blood vessels (arteries and veins) and lower your blood pressure. These medicines can reduce your heart's workload, help widen coronary arteries, and relieve and control angina.
* Nitroglycerin widens the coronary arteries, increasing blood flow to the heart muscle and relieving chest pain.
* Long-acting nitrates are similar to nitroglycerin but are longer acting and can limit the occurrence of chest pain when used regularly over a long period.
* Glycoprotein IIb-IIIa inhibitors are very strong antiplatelet medicines that are used in hospitals during and after angioplasty or to treat angina.
* Thrombolytic agents dissolve the clots that can occur during a heart attack. Thrombolytic therapy is administered in the hospital. Thrombolytic therapy and other treatments for heart attack are more effective the sooner they are given after a heart attack starts. You need to get to a hospital as soon as possible if you think you are having a heart attack.
Coronary Artery Surgery Special Procedures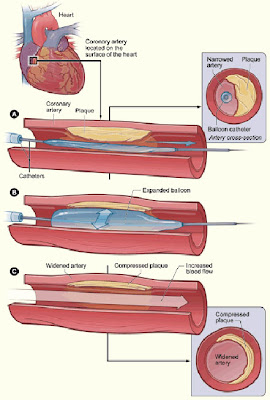
* Angioplasty. This procedure opens blocked or narrowed coronary arteries. It can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack. Sometimes a device called a stent is placed in the artery to keep the artery propped open after the procedure.
* Coronary artery bypass surgery. In this procedure arteries or veins from other areas in your body are used to bypass your narrowed coronary arteries. Bypass surgery can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
Angioplasty or bypass surgery may be used to treat CAD if:
* Medicines and lifestyle changes have not improved your symptoms.
* Your symptoms are getting worse.
Some people may need to have angioplasty or bypass surgery on an emergency basis during a heart attack to limit damage to the heart.
Cardiac Rehabilitation
Your doctor may prescribe cardiac rehabilitation (rehab) for angina or after bypass surgery, angioplasty, or a heart attack. Cardiac rehab, when combined with medicine and surgical treatments, can help you recover faster, feel better, and develop a healthier lifestyle.
Almost everyone with CAD can benefit from cardiac rehab.
Cardiac rehab often begins in the hospital after a heart attack, heart surgery, or other heart treatment. Rehab continues in an outpatient setting after you leave the hospital.
The cardiac rehab team may include:
* Doctors
o Your family doctor
o A heart specialist
o A surgeon
* Nurses
* Exercise specialists
* Physical therapists and occupational therapists
* Dietitians
* Psychologists or other behavior therapists
Rehab has two parts:
* Exercise training. This helps you learn how to exercise safely, strengthen your muscles, and improve your stamina. Your exercise plan will be based on your individual ability, needs, and interests.
* Education, counseling, and training. This helps you understand your heart condition and find ways to reduce your risk of future heart problems. The cardiac rehab team will help you learn how to cope with the stress of adjusting to a new lifestyle and to deal with your fears about the future.
For more information on cardiac rehab, consult "Recovering from Heart Problems Through Cardiac Rehabilitation: Patient Guide" from the Agency for Healthcare Research and Quality.
How Can Coronary Artery Disease Be Prevented or Delayed?
Preventing or delaying coronary artery disease (CAD) begins with knowing which risk factors you have and taking action. Remember, your chances of developing CAD increase with the number of risk factors you have.
Know your family history of health problems related to CAD. If you or someone in your family has CAD, be sure to tell your doctor. Make sure everyone in your family gets enough exercise and maintains a healthy body weight.
By controlling your risk factors with lifestyle changes and medicines, you may prevent or delay the development of CAD.
CAD can cause serious complications, but by following your doctor's advice and changing your habits, you can prevent or reduce the chance of:
* Dying suddenly from cardiac problems
* Having a heart attack and permanently damaging your heart muscle
* Damaging your heart because of reduced oxygen supply
* Having irregular heartbeats (arrhythmias)
Home Remedies and Alternative Therapies for Coronary Artery Disease
There is no substitute for medical care when considering a serious—even potentially fatal—condition such as coronary heart disease. The first thing to do if you notice any symptoms of a heart problem, including chest pain, is to see your doctor. Medical treatment may be required to prevent heart attack. However, your doctor may recommend nonmedical measures, such as:
* exercise conditioning,
* relaxation techniques such as yoga, and
* a low-fat diet.
These measures may help ease the symptoms of coronary heart disease, especially angina, and may help ease the effects of some risk factors. For example, relaxation techniques may help you overcome stress and block pain impulses by refocusing your concentration. These techniques include meditation, yoga, biofeedback training, and self-hypnosis. For maximum benefit, you should choose a relaxation technique that you are comfortable with and practice it for 20 minutes once or twice a day. In addition to the direct positive effect on your cardiovascular system, relaxation techniques may help you make other lifestyle changes such as stopping smoking and contribute to a general sense of well-being.
Vitamin therapy may also work in conjunction with your medical treatment. High doses of niacin can lower blood cholesterol levels, reducing the buildup of fatty deposits in the arteries. In addition, recent studies indicate that vitamin E, an antioxidant vitamin that also inhibits blood clotting, may help reduce the risk of heart attack. However, do not take any more than the Recommended Dietary Allowance (RDA) of any vitamin without first consulting your doctor; some vitamins in high doses can have toxic effects.
Other more controversial, alternative therapies include garlic, which may be consumed as deodorized pills, and fish oil (omega-3 fatty acid) supplements. Ongoing studies indicate that large amounts of garlic may have a modest cholesterol-lowering effect. Any benefits of fish oil supplements are offset by the increased calorie and fat intake. Thus, experts recommend eating one or two servings of salmon, cod, or other cold-water fish a week rather than taking fish oil pills.
Still other alternative therapies provide no benefit and should be avoided. These include chelation therapy, a technique used to remove heavy metals such as lead from the blood.
Saturday, May 19, 2007
Coronary Artery Disease | Coronary Heart Disease Causes, Symptoms and Treatments
Posted by
Feliciana
at
4:50 AM
![]()
![]()
Labels: Coronary Artery Causes, Coronary Artery Disease, Coronary Artery Symptoms, Coronary Artery Treatments, Coronary Heart Disease
Subscribe to:
Post Comments (Atom)












No comments:
Post a Comment